How being less deadly allowed COVID-19 to kill so many people
When the SARS epidemic first appeared in China and Hong Kong in 2002 and then began to spread internationally, there was no debate about our goal in managing the disease. SARS killed 10% of those infected and no one suggested anything other than the complete elimination of the disease and the particular coronavirus responsible. Within three years, SARS had been eradicated. Ironically, the far lower case-fatality rate of COVID-19, about 1%, has played a central role in making it so deadly. The fact that most cases are likely to survive inspired many politicians and public figures, and even a few epidemiologists, to contend that the Zero COVID strategy was just not worth it. The results are reported daily for all to see. 2.4 million dead. For comparison, Ebola, one of the most deadly diseases in history, killed 11,034. And how many died from SARS? 811.
How did we get this so completely wrong?
THE MASSIVE FAILURE OF LAISSEZ-FAIRE
The Lancet Commission on Public Policy and Health in the Trump Era just estimated that Trump’s policies could be blamed for 40% of the COVID-19 deaths. But there is a fundamental flaw in their assertion that Trump is responsible for almost 200,000 American deaths. The staggering number is wildly wrong. It is too low.
The authors of the Lancet study compared American death rates to those in other industrialized countries. The problem is that almost all of those countries got it wrong. We just got it more wrong. If Trump’s policies had been merely as bad as other industrialized countries, it could have cut American deaths dramatically. But what if we compare ourselves to countries that got it right? If we had simply matched the performance of Canada, we would have reduced deaths in the United States by 62%. But Canada didn’t get it right. Japan had a death rate 96% lower than the United States. And matching top performing countries like New Zealand, Vietnam, or Taiwan would have saved over 485,000 American lives.
What did these countries do differently? Setting asides the details, the basic answer is simple.
From the very start, they had a single goal. Zero COVID.
Herd Immunity through infection is not a strategy
Bizarrely, outside of the few truly successful countries, the idea of aspiring to eliminate COVID-19 has become radical fringe idea. In fact, many have suggested that we would be better off if we allowed the spread of the disease among younger age groups because they are less likely to experience severe disease and that the immunity they would acquire as a result would limit the subsequent spread of the disease. The idea of increasing the percent of the population that is resistant to a disease to control it is not new. Herd immunity lies at the heart of infectious disease control. But the centerpiece of herd immunity has always been vaccination. Never before has anyone in public health sought to control a serious disease by allowing the disease to spread. In fact, public health experts have a term to describe reaching herd immunity through active infection.
Failure.
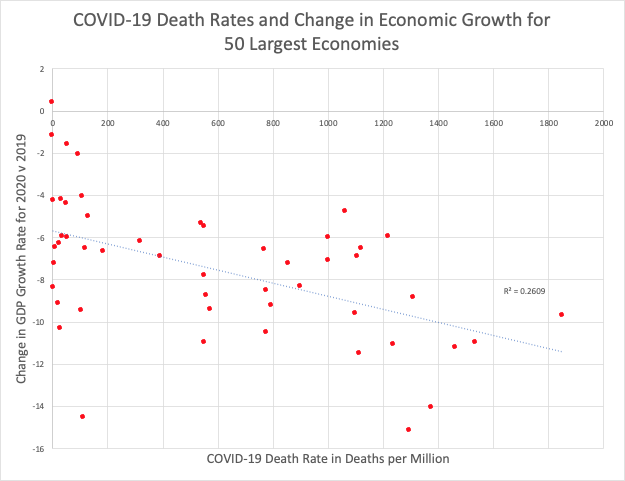
UNMASKING THE ECONOMIC ARGUMENT
What is so wrong about the strategy of letting the disease spread in less vulnerable segments of the population? There are two major problems. The first is simple. It doesn’t work. Not only do countries and regions that tilted towards the lax restrictions aimed at disease generated herd immunity have some of the highest rates of cases and deaths related to COVID-19, their economies did significantly worse as COVID-19 death rates rose. Globally, economic growth for 2020 fell sharply as compared to 2019. Second, the herd immunity strategy implicit in the Great Barrington Declaration may ultimately make it harder to achieve herd immunity with a vaccine. To understand this seeming paradox, we need to look at how the virus changes over time.
The risk of replication
A case study of a single man, originally released in December, provides a dramatic example of why every case matters. The man, who had a severe auto-immune disease that required immunosuppressive therapy, became infected with COVID. In other words he had an immune system that was active, but incapable of eliminating the virus. As a result, in the course of one infection, the virus accumulated a cluster of 20 mutations and created a strain similar to the UK variant. This is a microcosm of what we are doing when we seek herd immunity by infection.
In other words, every replication of SARS-COV-2 puts vaccine efficacy at risk. In the course of a single infection, each virus in the initial infectious dose typically produces many millions of copies of itself. More cases=more mutations= more risk. We must use the best available measures to minimize the number of cases of COVID-19. Otherwise, we risk the emergence vaccine resistant SARS-COV-2.
More cases=more mutations= more risk.
Letting COVID-19 spread while we slowly roll out a vaccine, is like a person with a bacterial infection taking antibiotics at too low a dose. It won’t kill all the bacteria and the ones that remain will be those with some capability to resist the antibiotic. In the case of this man, instead of antibiotics, the virus was resisting the human immune system. Every time a person develops COVID-19, those virus strains most capable of replicating and transmitting infection to others will be selected. As time goes on, these new variants will look less and less like the virus used as the model for existing vaccines.
Zero covid is not a radical concept
So, how do we achieve zero-COVID. Let’s look at the strategy of those countries have successfully pursued this approach.
- Masks:
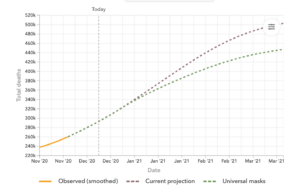
Masks work. In fact, universal use of well-fitting masks is almost as effective as the best vaccine in preventing the spread of COVID-19. The countries most successful in stopping spread had near universal use of masks. Mandatory mask use will be central to any zero-COVID strategy. - Lockdowns:
The anti-lockdown rhetoric is deeply flawed and dangerous. This is a disease that spreads through human interaction. If people don’t go out, the disease won’t spread. A well executed lockdown could eliminate the disease in less than five weeks. Two weeks to identify anyone in a home that might be infected. An additional two weeks to ensure there is no secondary spread among household members from asymptomatic cases. And done. That was at the core of the New Zealand’s strategy. It worked. - Testing:
Frequent, inexpensive testing, as advocated by Dr. Michael Mina, could identify the most infectious cases before they expose anyone. Coupling pre-emptive testing with a thoughtfully considered lockdown strategy and ongoing vaccination will be a key part of a Zero-COVID strategy. - Travel Restrictions:
Once the cases within a region have been eliminated, the only source of new cases will be travelers. That means that inbound as well as returning travelers will need to be tested and quarantined. This is particularly daunting for non-island states and nations, but Germany is actively addressing this challenge. - Contact Tracing:
Zero COVID is a goal. Until all regions of the world have it under control, cases will emerge. It is essential that aggressive contact tracing along with quarantine be used to eliminate the potential for outbreaks to spread.
This is all basic epidemiology (the kind they teach to actual epidemiologists). We simply need to do it. That requires enlightened political leadership, an educated and morally responsible public, and the understanding that getting to zero-COVID is not a radical concept.
It is common sense.


One THOUGHTS ON “We Dismissed Zero COVID. Now We Have a Double Disaster.”
Comments are closed